Clomiphene Citrate, Overlooked Testosterone Replacement Therapy (TRT) Alternative? 2.5x Higher T, No Side Effects
While many of the things people will tell you about the negative side-effects of testosterone replacement therapy (TRT) are scientifically questionable, un- or even disproven, there’s one nasty side effect that is simply unavoidable: the decline in natural testosterone production. Needless to say that this is why natural testosterone boosters, i.e. products that contain (natural) ingredients that may boost your own endogenous testosterone production, are so popular. Unfortunately, these pills have a larger impact on their manufacturers revenue than your T-levls. If they even work, the meager 20%-30% T increase they have to offer is simply not enough for someone whose testosterone level hovers at
It’s not enough to bring someone with a low testosterone production back into the normal or upper normal range; the place, where all of us would like to be – and that’s exactly, where studies indicate clompiphene citrate may come in.
10 years ago, Shabsigh and his colleagues from the NY Presbyterian Medical Center investigated the effects of 25mg of clomiphene citrate per day in 36 Caucasian men with hypogonadism )defined as serum testosterone level less than 300 ng/dL).
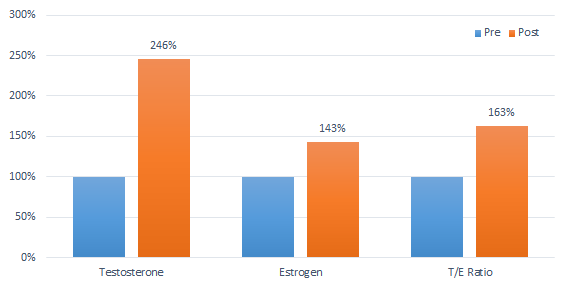
Figure 1 : Pre-/post testosterone, estrogen and T/E ratio in the 27-60-year old subjects before and after taking a low dose of 25mg clompiphene citrate per day for 4-6 weeks (Shabsigh. 2005) | the bars in the graph show relative values (control = 100%), the figures on top are absolute values in the units shown below each bar).
As you can see in Figure 1, the testosterone levels of the 27-60-year old subjects, which were 247.6 ± 39.8 ng/dL respectively, had risen by a whopping 146% to 610.0 ± 178.6 ng/dL at the first follow-up visit (4–6 weeks). Due to the fact that SERMs are recognized as estrogens by the body, the aromatase from testosterone to estrogen didn’t increase to the same extent. Accordingly, the T/E ratio improved as well – from 8.7 to 14.2 (P < 0.001 | that’s 60.9%), to be specific.
What is clomiphene citrate? Clomiphene citrate is a selective estrogen receptor modulator that was developed to stop estrogen dependent breast cancer growth. The way the molecule binds to the estrogen receptor without fully initiating the pro-estrogenic signalling cascade is yet also interesting for men, because in men estrogen is the #1 negative feedback factor. This means when estrogen levels are high and the receptors in the brain are free to dock to, your body will think “hmm… if there’s so much estrogen floating around and estrogen can only be produced (in men) if its derived from testosterone by aromatization, there must be plenty of testosterone, so let’s shut down the production.” Well, ok, that’s not a scientifically accurate description, but I guess you get how it works. If the SERM blocks the receptor the negative feedback is shut down and the testosterone production can flourish.
Very similar results were observed in a cohort of 990 men who presented with sexual dysfunction who received a similar total dose of clomiphene citrate, but as 50mg taken every other day. What is particularly interesting about this, study, though, is that (a) not all subjects even had “low” (by definition) T-levels and that (b) the restoration of normal or even normal-high testosterone levels did not, as some of you may expect, restore the subjects messed up sexual function. Especially in the older subjects, other organic reasons (e.g. atherosclerosis, diabetes, etc.) may have blunted the beneficial effects of T.

Figure 2: Effect of 50mg clomiphene citrate eod on sexual function (responder = restored, etc.) stratified for age (left) and testosterone response stratified (right | Guay. 2003)
That’s not enough? Well, almost identical results have been reported by Ioannidou-Kadis (2005), Whitten (2006) and Kaminetsky et al. (2009 & 2013); and Hussein et al. (2005) even recommend clomiphene citrate administration for cases of nonobstructive azoospermia.
Now you will probably be asking for side effect, right? Well, all of the previously cited studies report none of the often heard of side effects that occur on the high doses in post-cycle therapy of steroid using athletes like distorted vision or impaired blood lipids. And a 2012 study by Moskovic et al. found no physiological or psychological side effects, either. That’s why I wouldn’t overrate either the reports of debilitating physiological side effects on the boards or the three existing case reports about psychotic episodes in men with pre-existing psychological issues on clompiphene citrate (Knight. 2015).

Table 1: While the testosterone levels will increase even if you’re sick (having diabetes and hypertension) the beneficial effects on sexual function are blunted in men with endothelial or metabolic disease (Guay. 1995).
What I would take into consideration, though is the following caveat: Clomiphene works only in men whose natural testosterone production is still intact. If your T-levels are low, because there’s a physiological problem with your testes (as it often occurs when you age | Tenover. 1991) or hypothalamus, it won’t work, because even if clomiphene takes away the negative feedback estrogen exerts in the “hormone production control center” in your brain, this will increase the T- production onl if the “center” and your testes are both functioning properly.
So what? Is it an alternative? Well, let me cite Frederick Taylor and Laurence Levine who compared clomiphene citrate (CC) and regular testosterone gel replacement therapy (TGRT) in their 2010 study and conclude that “CC represents a treatment option for men with hypogonadism, demonstrating biochemical and clinical efficacy with few side effects and lower cost as compared with TGRT” (Taylor. 2010). And that’s not all, clomiphene citrate was cheaper (83$ vs. $265 per month) and again, “[t]here were no adverse events reported” (Taylor. 2014) in any patients at the 8–40 month follow ups. What remains to be sees is what will happen if you’re “on” for 10 years.
CC will yet only work if your testes & HPT work. Otherwise, TRT is is the only option to get back to normal testosterone levels. For people whose T levels are suppressed for other reasons (e.g. steroid abuse | Figure 3), it’s a viable alternative – in the medium to short run |
Figure 3: While clomiphene won’t help people who don’t produce enough testosterone because their testes or hypthalamus are malfunctioning, there’s good evidence, for example from a 2012 study by Katz et al., that proves that it will restart the endogenous testosterone production of chemical athletes (Katz. 2010).
References:
Guay, ANDRE T., S. U. D. H. I. R. Bansal, and GERALD J. Heatley. “Effect of raising endogenous testosterone levels in impotent men with secondary hypogonadism: double blind placebo-controlled trial with clomiphene citrate.” The Journal of Clinical Endocrinology & Metabolism 80.12 (1995): 3546-3552.
Guay, A. T., et al. “Clomiphene increases free testosterone levels in men with both secondary hypogonadism and erectile dysfunction: who does and does not benefit?.” International journal of impotence research 15.3 (2003): 156-165.
Hussein, Alayman, et al. “Clomiphene administration for cases of nonobstructive azoospermia: a multicenter study.” Journal of andrology 26.6 (2005): 787-791.
Ioannidou-Kadis, Stella, et al. “Complete reversal of adult-onset isolated hypogonadotropic hypogonadism with clomiphene citrate.” Fertility and sterility 86.5 (2006): 1513-e5.
Moskovic, Daniel J., et al. “Clomiphene citrate is safe and effective for long‐term management of hypogonadism.” BJU international 110.10 (2012): 1524-1528.
Kaminetsky, Jed, and Micah L. Hemani. “Clomiphene citrate and enclomiphene for the treatment of hypogonadal androgen deficiency.” Expert opinion on investigational drugs 18.12 (2009): 1947-1955.
Kaminetsky, Jed, et al. “Oral enclomiphene citrate stimulates the endogenous production of testosterone and sperm counts in men with low testosterone: comparison with testosterone gel.” The journal of sexual medicine 10.6 (2013): 1628-1635.
Katz, Darren J., et al. “Outcomes of clomiphene citrate treatment in young hypogonadal men.” BJU international 110.4 (2012): 573-578.
Knight, Julia C., et al. “Clomiphene-Associated Suicide Behavior in A Man Treated for Hypogonadism: Case Report and Review of The Literature.” Psychosomatics (2015).
Shabsigh, Ahmad, et al. “Clomiphene citrate effects on testosterone/estrogen ratio in male hypogonadism.” The journal of sexual medicine 2.5 (2005): 716-721.
Tan, Robert S., and Deepa Vasudevan. “Use of clomiphene citrate to reverse premature andropause secondary to steroid abuse.” Fertility and sterility 79.1 (2003): 203-205.
Taylor, Frederick, and Laurence Levine. “Clomiphene citrate and testosterone gel replacement therapy for male hypogonadism: efficacy and treatment cost.” The journal of sexual medicine 7.1pt1 (2010): 269-276.
Tenover, Joyce S., and William J. Bremner. “The Effects of Normal Aging on the Response of the Pituitary‐Gonadal Axis to Chronic Clomiphene Administration in Men.” Journal of andrology 12.4 (1991): 258-263.
Whitten, Scott J., Ajay K. Nangia, and Peter N. Kolettis. “Select patients with hypogonadotropic hypogonadism may respond to treatment with clomiphene citrate.” Fertility and sterility 86.6 (2006): 1664-1668