Written by Dr. Datis Kharrazian
Science has reliably proven that environmental pollutants, chemicals, and toxins can trigger autoimmunity. These chemicals include mercury, lead, benzene, solvents, and other compounds found in our everyday environment — carpets, mattresses, plastic utensils, plastic water bottles, fire retardants found in furniture and children’s pajamas, etc.
Many people mistakenly believe the best thing to do in the face of so many toxic burdens is to undergo chelation, a process that pulls metals and chemicals out of the body. In this article I’ll talk about why that is dangerous, especially if you have autoimmunity, chemical sensitivities, or symptoms of compromised brain function. Chelation often makes people much worse, and it is not due to a “detox reaction” as many practitioners will tell you.
Why toxins trigger autoimmunity in some and not others
It has become impossible to completely avoid environmental toxins no matter where you live. These toxins are now in our oceans, rivers, lakes, groundwater, rainwater, and air. They are found in our soil throughout the world, including in the soil that grows organic foods. Chemicals in produce cannot be washed or peeled away as they bind to proteins in the plant while it’s growing.
Research indicates most of us have elevated levels of chemicals and heavy metals in our bodies these days. Studies are showing increasing levels of chemicals in fetal tissue, human milk, and other bodily tissues. (1-3)
So if we’re all carrying around a toxic burden, why do environmental chemicals triggers multiple chemical sensitivities, autoimmunity, and other chronic health issues in some people and not others?
The issue is not how many chemicals or heavy metals a test shows are in your body but whether your immune system is reacting to these environmental compounds. You can react to a toxin the same way you can react to a food, such as gluten or dairy.
In fact, research I conducted with Dr. Aristo Vojdani showed approximately 20 percent of normal, healthy people demonstrate immune reactivity to chemicals. We published this research in the Journal of Applied Toxicology, which you can access free here.
The review board for this study called it “revolutionary” and “breakthrough research.” It is the first study that shows a completely new model of how chemicals combine with our own proteins to create autoimmunity and how prevalent this is in our population. And we are still finding correlations between immune reactivity to chemicals and various autoimmune reactions. We will publish those findings in the coming months.
So elevated levels of heavy metals or chemicals on a hair analysis or other test do not tell the whole story. What matters is whether your immune system is reacting to these compounds and NOT the quantity or levels you have.
How environmental chemicals lead to autoimmunity
Research shows three key factors act together in triggering autoimmunity:
1) First, you must be exposed to chemicals, which we all are.
2) Second, these chemicals must bind to our own tissue proteins creating new antigens (an antigen is any substance that causes your immune system to produce antibodies against it, tagging it for destruction and removal). This immune reaction cannot occur against the chemical itself. The chemical must be attached to a protein in a tissue in your body for an immune reaction to occur.
3) Third, we have an immune reaction to the chemical bound to the protein, which the immune system recognizes as an antigen.
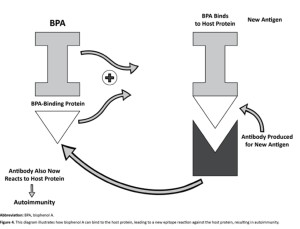
In the illustration here, we have BPA (bisphenol A, which is found in many plastic products) binding to human tissue. For instance, BPA has been shown to have an affinity for binding to human albumin. Once it is bound to the tissue, that tissue now appears as a foreign antigen to the immune system, which tags it with antibodies for destruction and removal. Thus begins or triggers the autoimmune process in some individuals. For a more detailed version of this chemical model please refer to my paper published in the scientific journal Autoimmune Disease.
The risks and dangers of chelation therapy when you have autoimmunity or compromised brain function
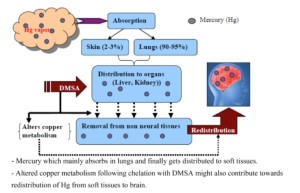
When a person with chemical sensitivities or a chronic health issue comes into a practitioner’s office, many run tests for heavy metals and environmental chemicals, which always come back positive. Virtually everyone tests for high levels of chemicals, especially with a challenge test. The person is then chelated using DMSA, DMPS, or EDTA. Any adverse reactions are dismissed as a detox reaction. But the truth is chelation can be devastating to those with autoimmunity, neurodegeneration (the brain is degenerating too fast), or an immune reactivity to chemicals.
Chelation can be dangerous when you have autoimmunity. I have seen chelation therapy destroy people’s health. If you have an immune reaction to chemicals causing autoimmunity and you undergo chelation you could make a bad situation many times worse.
Research has clearly demonstrated that chelation pulls heavy metals out of body tissue and redistributes them so that they make their way into the brain, promoting toxicity, inflammation, neurodegeneration, and sometimes serious side effects. (1-7)
The decision to undergo chelation therapy should not be taken lightly. Since most practitioners do not understand the risks I will explain the basic concepts about knowing when chelation is safe.
What you need know if you are considering chelation
If you are considering chelation therapy you MUST establish whether you have “chemical tolerance.” Chemical tolerance means the immune system has the ability to respond appropriately to compounds such as toxins, pollutants, and dietary proteins – that these compounds do not trigger an immune reaction. Of course, certain toxins are immediately poisonous to everyone, such as certain mushrooms, Agent Orange, high-level radiation, etc. However, many chronically ill people cannot tolerate relatively benign exposures, such as perfumes, detergents, jewelry, etc. This is because they have lost their chemical tolerance.
Source: Int J Environ Res Public Health. Jul 2010; 7(7): 2745–2788
Loss of chemical tolerance
Symptoms of loss of Immune-Chemical Tolerance
- Intolerance to smells
- Intolerance to jewelry
- Intolerance to shampoo, lotions, detergents, etc.
- Multiple food sensitivities
- Constant skin outbreaks
The loss of chemical tolerance is a phenomenon both researchers and clinicians have identified in more than a dozen countries and across diverse groups of people. These are the people for whom gas fumes, scented body products, laundry detergents, fabric softeners, new carpeting, new construction, new car smell, and so on trigger such symptoms and conditions, including asthma, migraines, depression, fibromyalgia, fatigue, Gulf War syndrome, brain fog, memory loss, incontinence, neurological dysfunction, rashes, their particular autoimmune symptoms, and so on.
A variety of factors can contribute to loss of chemical tolerance:
- Regulatory T-cell integrity. Regulatory T-cells are immune cells that regulate and balance the immune system and prevent autoimmunity or loss of chemical tolerance.21 They are key in preventing a TH-1 or TH-2 dominance. Glutathione depletion causes loss of regulatory T-cell function, as do deficiencies in vitamin D and omega-3 fatty acid.
- Antioxidant reserves. Depletion of glutathione, the body’s master antioxidant, is a primary cause of loss of chemical intolerance. Everyday levels of environmental compounds do not become an immune trigger unless the body’s glutathione levels are depleted. Glutathione depletion is also a major contributing factor to leaky gut, a leaky blood-brain barrier, and even leaky lungs.
- Barrier system integrity. Do you have a leaky gut or a leaky blood brain barrier? Many dietary and lifestyle factors can break down these immune barriers, increasing the risk for both loss of chemical intolerance and autoimmunity.
- Integrity of hepatic biotransformation pathways. Are your liver detox pathways functioning properly? Although the liver can’t break down many environmental compounds, proper liver function is still vital. If the liver detox pathways are not working properly it can add to the toxic burden. I talk more about this in my book Why Isn’t My Brain Working?
Some common complaints can compromise these systems and lead to loss of chemical tolerance. For example, chronic inflammation is a major predisposing factor in loss of chemical tolerance. It contributes to glutathione depletion, loss of immune barrier integrity, and poor regulatory T-cell function. Some common symptoms of chronic inflammation include bloating, skin rashes or eruptions, joint pain, brain fog, depression and anxiety, chronic pain, chronic fatigue, and autoimmune flare-ups.
Chronic stress is another contributing factor as it can break down the gut and brain barriers and create an insufficiency of immune regulatory T-cells.
And, of course, chemicals themselves can lead to loss of chemical tolerance by contributing to the breakdown of the body’s self-defense mechanisms. For instance, low concentrations of mercury have been shown to disrupt immune function and influence the risk of autoimmunity. Polychlorinated biphenyls (PCBs) have been banned but are still found in the environment and have been shown to break down the blood-brain barrier and gut barrier. Chronic exposure to arsenic in drinking water breaks down the lung barrier. Chronic toxic exposure can deplete the glutathione system. These are just a few examples of the ways environmental chemicals attack our self-defense systems, making us more vulnerable to loss of chemical tolerance.
The stages of loss of chemical tolerance
Loss of chemical tolerance appears to evolve in two stages. The first stage is characterized by a breakdown in the body’s natural tolerance to chemicals and heavy metals. In the second stage, an ordinary exposure to an environmental compound, whether it is traffic exhaust, fragrances, a drug, or other chemical, suddenly triggers an immune response.
I know of one woman in her 30s who had long suffered mild sensitivities to chemicals but it suddenly became severe when she stayed at a relative’s home that was heavily scented from commercial laundry products. She became dizzy as soon as she entered the home. While staying the night, she experienced the most severe vertigo of her life. By the time she made it home by plane (which was likely sprayed with an insecticide), she struggled with severe fatigue for the next two months and was largely confined to her bed. She went on to develop symptoms of MS, including loss of strength and motor function in her arms and legs when exposed to scented products or industrial fumes. Today, she must largely stay at home and eat a very strict diet to avoid a flare up. As a mother of four in her 30s, this has been an incredible hardship.
This is an example of an immune response leading to a profound breakdown of immune function. Many of these people go on to develop multiple chemical sensitivities (MCS), severe allergies, multiple food intolerances, and autoimmunity. Loss of chemical tolerance increasingly shrinks not only their world but also their diet as they react to a growing list of foods. Managing their cases can be difficult as many herbs and supplements trigger reactions.
Many of us may be just one major stress event away from losing chemical tolerance. It can be an IRS audit, a divorce, a lawsuit, a car accident, or other trauma. It is important for individuals to maintain their immune health and shore up their defenses so they are better able to withstand daily chemical assaults and the occasional crises life delivers.
Once individuals lose their chemical tolerance, they can develop a variety of other health conditions, such as headaches, depression, asthma, chronic fatigue, fibromyalgia, autoimmunity, etc. Many do not realize that the chemicals in their environment are triggering their chronic immune reactions.
How to know whether it’s safe to chelate
If you have symptoms of loss of chemical tolerance you should be very cautious of chelation therapy. Below are the concepts I use with my patients. For the best outcomes, you may need to work with a competent practitioner who understands these concepts. You can look for a functional medicine practitioner here.
- Despite the quantity of heavy metal compounds that showed up on your standard heavy metal test, you need to order the Cyrex Array 11 Chemical Immune Reactivity Screen. This will tell you whether you are having an antibody reaction to any of the chemicals, which indicates you have lost chemical immune tolerance. If any markers on the test come back positive, do not consider chelation therapy, especially if you are reacting to heavy metals. You should never consider chelation until the test shows your antibody reactions are normal.
- Evaluate the integrity of your blood-brain barrier with the Cyrex Array 20 Blood Brain Barrier Permeability test. If it is positive, refer to the nutritional strategies in my book Why Isn’t My Brain Working?, particularly in the chapter on brain inflammation.
- Evaluate for intestinal permeability, or leaky gut, with the Cyrex Array 2 Intestinal Antigenic Permeability Screen and manage with diet, nutrition, and lifestyle. I discuss those strategies in both my thyroid and brain books.
- Increase your glutathione levels and glutathione recycling with compounds that support that, such as milk thistle, N-acetyl cysteine, Cordyceps, Gut Kola Extract, S-acetyl-glutathione, etc. For more information, refer to my brain book.
- Consider a detoxification program with diet, nutrition, and botanical support. Refer to the chapter on toxins and the brain in my brain book.
- After following the protocols, re-evaluate your status with the laboratory profiles to determine whether the chemical immune reactivity, blood-brain barrier and intestinal permeability issues are resolving. Do not proceed with chelation until these tests show your barriers are intact and you’re not reacting to chemicals or metals.
Disclaimer: Dr. Datis Kharrazian is a paid consultant to Cyrex Labs and serves on their Scientific Advisory Board.
References on Chemical Burden
1. Li LX, Chen L, Meng XZ, Chen BH, Chen SQ, Zhao Y, Zhao LF, Liang Y, Zhang YH. Exposure levels of environmental endocrine disruptors in mother-newborn pairs in China and their placental transfer characteristics. PLoS One. 2013 May 7;8(5):e62526.
2. Barr DB, Bishop A, Needham LL. Concentrations of xenobiotic chemicals in the maternal-fetal unit. Reprod Toxicol. 2007 Apr-May;23(3):260-6.
3. Zhao G, Xu Y, Li W, Han G, Ling B. PCBs and OCPs in human milk and selected foods from Luqiao and Pingqiao in Zhejiang, China. Sci Total Environ. 2007 Jun 1;378(3):281-92.
References on Chelation Redstribution:
1. Andersen O. Chemical and biological considerations in the treatment of metal intoxications by chelating agents. Mini Rev Med Chem. 2004 Jan;4(1):11-21.
2. Ewan KB, Pamphlett R. Increased inorganic mercury in spinal motor neurons following chelating agents. Neurotoxicology. 1996 Summer;17(2):343-349.
3. Ibim SE, Trotman J, Musey PI, Semafuko WE. Depletion of essential elements by calcium disodium EDTA treatment in the dog. Toxicology. 1992;73(2):229-237.
4. Flora SJ, Pachauri V. Chelation in metal intoxication. Int J Environ Res Public Health. 2010 Jul;7(7):2745-2788.
5. Andersen O. Principles and recent developments in chelation treatment of metal intoxication. Chem Rev. 1999 Sep 8;99(9):2683-2710.
6. Andersen O. Chemical and biological considerations in the treatment of metal intoxications by chelating agents. Mini Rev Med Chem. 2004 Jan;4(1):11-21.
7. Ewan KB, Pamphlett R. Increased inorganic mercury in spinal motor neurons following chelating agents. Neurotoxicology. 1996 Summer;17(2):343-349.
References for Immune Chemical Tolerance
1. Cranor C. The legal failure to prevent subclinical developmental toxicity. Basic Clin Pharmacol Toxicol. 2008 Feb;102(2):267-273.
2. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 Dec 15;380(9859):2224-60.
3. Agency for Toxic Substances & Disease Registry. Priority LIst of Hazardous Substances That Will Be the Subject of Toxicological Profiles. http://www.atsdr.cdc.gov/SPL/index.html. Updated October 25, 2011. Accessed March 4, 2013.
4. Miller CS. The compelling anomaly of chemical intolerance. Ann N Y Acad Sci. 2001 Mar;933:1-23.
5. Requejo R, Tena M. Influence of glutathione chemical effectors in the response of maize to arsenic exposure. J Plant Physiol. 2012 May 1;169(7):649-656.
6. Vojdani A, Lambert J. The onset of enhanced intestinal permeability and food sensitivity triggered by medication used in dental procedures: a case report. Case Rep Gastrointest Med. 2012;2012:265052.
7. Mićović V, Vojniković B, Bulog A, Coklo M, Malatestinić D, Mrakovcić-Sutić I. Regulatory T cells (Tregs) monitoring in environmental diseases. Coll Antropol. 2009 Sep;33(3):743-746.
8. Winder C. Mechanisms of multiple chemical sensitivity. Toxicol Lett. 2002 Mar 10;128(1-3):85-97.
9. Gardner RM, Nyland JF, Evans SL, et al. Mercury induces an unopposed inflammatory response in human peripheral blood mononuclear cells in vitro. Environ Health Perspect. 2009 Dec;117(12):1932-1938.
10. Seelbach M, Chen L, Powell A, et al. Polychlorinated biphenyls disrupt blood-brain barrier integrity and promote brain metastasis formation. Environ Health Perspect. 2010 Apr;118(4):479-484.
11. Choi YJ, Seelbach MJ, Pu H, et al. Polychlorinated biphenyls disrupt intestinal integrity via NADPH oxidase-induced alterations of tight junction protein expression. Environ Health Perspect. 2010 Jul;118(7):976-981.
12. Olsen CE, Liguori AE, Zong Y, Lantz RC, Burgess JL, Boitano S. Arsenic upregulates MMP-9 and inhibits wound repair in human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2008 Aug;295(2):L293-L302.
13. Genuis SJ. Sensitivity-related illness: the escalating pandemic of allergy, food intolerance and chemical sensitivity. Sci Total Environ. 2010 Nov 15;408(24):6047-6061.
14. Genuis SJ. Sensitivity-related illness: the escalating pandemic of allergy, food intolerance and chemical sensitivity. Sci Total Environ. 2010 Nov 15;408(24):6047-6061.